As with everything else, ICU management of sepsis should ideally the evidence based. Evidence based practice combines the best scientific knowledge (evidence) with patient preferences and clinical assessment and judgement.
While the pursuit of specific pharmaceutical agents to treat Sepsis has resulted in the expenditure of billions of dollars without producing a single effective agent, much of what we do in the treatment of patience with Sepsis can be evidence based. Clinicians make literally hundreds of decisions day on the management of an individual patient in the ICU, often these decisions are made routinely without a great deal of thought about the reasoning behind them. Every decision made about the treatment of a critically ill patient should be based on evidence or the belief that the action resulting from that decision will improve a patient centred outcome for that particular patient. A patient centred outcome is an outcome that affects how the patient feels, functions or survives meaning we should question every decision we make to ask whether it is going to improve one of those outcomes.
The best evidence on which to base of such decisions comes from large robust randomised controlled trials conducted by unbiased investigators. The last 20 years has seen the emergence and maturing of regional and national clinical trials groups who conduct such studies and increasingly collaborate with each other. (2) Such collaboration is often essential to perform studies large enough to provide evidence to guide clinical practice such collaboration is often essential to perform studies large enough to provide evidence to guide clinical practice. As someone who designs and contacts clinical trials I am well aware that they provide evidence on a population basis. Each trial result is the net of harm and benefit resulting from the treatment being studied and even when a treatment is proven to have a net benefit there may be some patients who are harmed by the use of that treatment. A graphic example of this is someone who suffers a massive intracranial haemorrhage when treated with thrombolysis. Causing visible harm to a patient may shake a clinician’s faith in an effective treatment making it important that we accept such tragic events without changing our practice to deny that effective treatment to future patients.
Research, like clinical practice, has inherent imperfections. Researchers, like clinicians, need to recognise this and be prepared to put their hand up and admit when they have been wrong. Conducting robust studies of appropriate size in an effective collaborative research group is the best way to avoid being wrong too often!
This podcast is presented by Pfizer
Pfizer has supported CODA 22 with an educational grant to support Coda Cure: Sepsis, Pandemics, Trauma & Communicable Diseases.

Simon Finfer
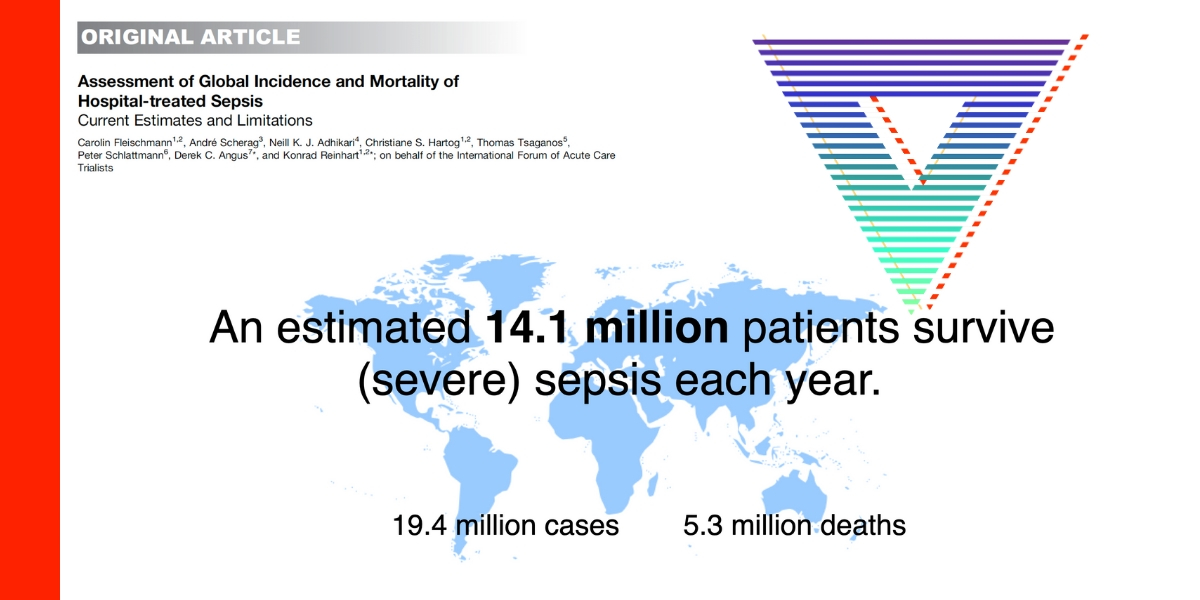
Simon Finfer is a Pom who emigrated to Australia in 1993 to practice full time intensive care medicine. Despite being qualified 37 years and receiving a small NHS pension he still works as a bedside clinician and takes night calls. He loves his job because he works with fantastic people. He also designs and runs large clinical trials, writes papers and edits books. His current mission is to reduce the global burden of sepsis to which end he sits on the Board of the Global Sepsis Alliance, the Council of the International Sepsis Forum and established both the Australian Sepsis Network and the Asia Pacific Sepsis Alliance. He is a Professorial Fellow at The George Institute for Global Health and the Institute’s focus on equity and improving the health of underserved populations in both rich and poor countries aligns perfectly with his and with CODA. Simon lives on the outskirts of Sydney with his wife, sons, three horses, four chickens, three ducks and one dog.