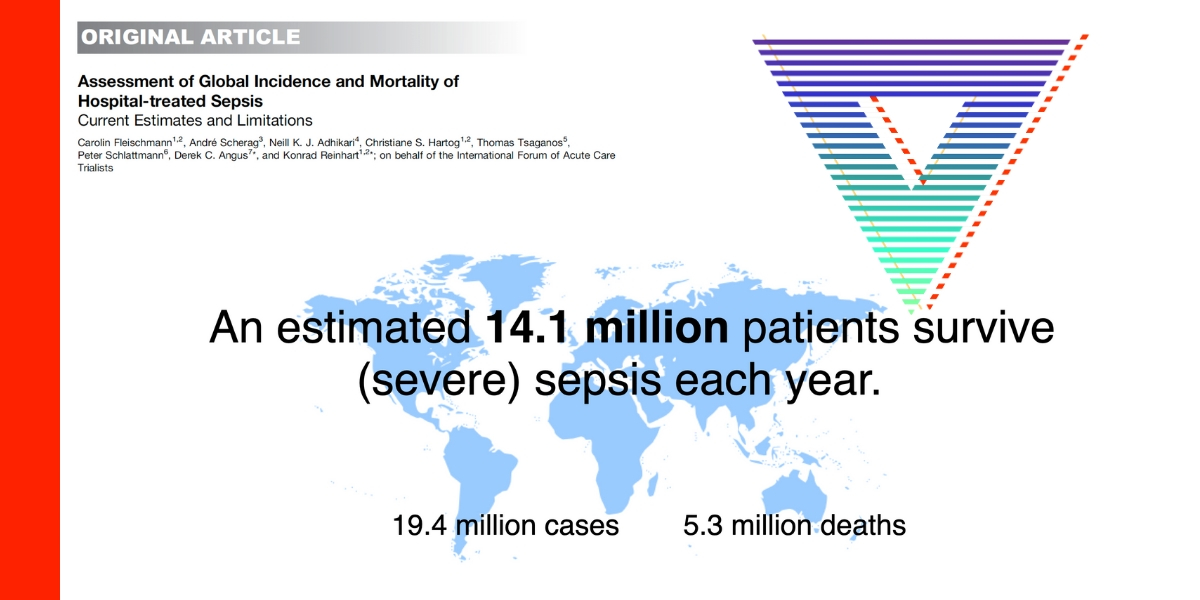
Sepsis in other words ‘life-threatening organ dysfunction’ in response to infection is a leading cause of death worldwide and a global health priority recognised by the World Health Organisation. In Australia, for adults with sepsis admitted to the intensive care unit, the in-hospital mortality is estimated as 18–27%. Early recognition of sepsis, prompt administration of antibiotics and resuscitation with intravenous fluids for those with features of hypo-perfusion or shock are the mainstays of initial treatment. Emergency departments often being the first point of contact for patients presenting with sepsis, are required to prioritise sepsis as a medical emergency. The “Sepsis Kills” program implemented across the nation aims to reduce unwarranted clinical practice variation in management of sepsis.
In a recent Australian based study conducted across four emergency departments in Western Sydney Local Health District, among 7533 patients with suspected infection, a reduction in risk of in-hospital mortality was observed for each 1000 mL increase in intravenous fluids administered in patients with septic shock or admitted to ICU. However, despite evidence showing mortality benefits, not all aspects of sepsis care have been given the needed attention. In the same setting, out of 4146 patients with sepsis, 45% of them did not receive intravenous fluids in the emergency departments within the first 24 hours. Younger patients with greater severity of illness and presented to smaller hospitals were more likely to receive fluids.
The unanswered questions regarding the facilitators and barriers influencing intravenous fluid administration in sepsis are being explored using qualitative methods. Several emergency physicians and nurses have provided insight into aspects that influence their ability to provide appropriate fluid resuscitation such as constantly overcrowded emergency departments with chronic staff shortages of skilled health professional, failure to recognise sepsis early, the complexity of the presentations and lack of resources. Awareness of these challenges among stakeholders is the need of the hour. Leaving no one behind and not disregarding the critical aspects of sepsis care are crucial. Recognition of these factors and sustainable interventions are necessary to improve clinical outcomes for patients.
For more head to our podcast page #CodaPodcast
This podcast is presented by Pfizer
Pfizer has supported CODA 22 with an educational grant to support Coda Cure: Sepsis, Pandemics, Trauma & Communicable Diseases.