Managing ICP in Traumatic Brain Injury: David Menon
David Menon discusses the complex and fraught world of managing traumatic brain injury (TBI) in the ICU.
In particular, David discusses the management of intracranial pressure and cerebral perfusion pressure in these patients.
Although the Brain Trauma Foundation provides guidelines for the management of severe TBI, including targets for ICP and CCP, there is no Level 1 recommendation for the use of any intervention to modulate ICP/CCP. General principles remain simple in theory, if not in practice.
David describes good basic intensive care, which he describes as doing lots of little things well.
The main focuses should be maintaining blood pressure high enough to get oxygen to brain, optimising oxygenation and modulating carbon dioxide.
This is in combination with other modalities such as hypertonic saline, cooling people, and using metabolic suppression. The trouble lies in the fact that there is no evidence base for second line therapy.
In fact, some of these therapies have been shown to cause harm. When considering a therapy, it boils down to this – is the disease desperate enough and have the benefits and risks of therapy been weighed up. When controlling ICP, the indications for treatment are different so acceptance of iatrogenic risk must also change.
Therefore, ICP treatments must be calibrated using a risk benefit ratio. For instance, utilising hyperventilation to decrease intracranial pressure can be a useful lever to pull. However, going too hard can reduce the cerebral blood flow to a detrimental point.
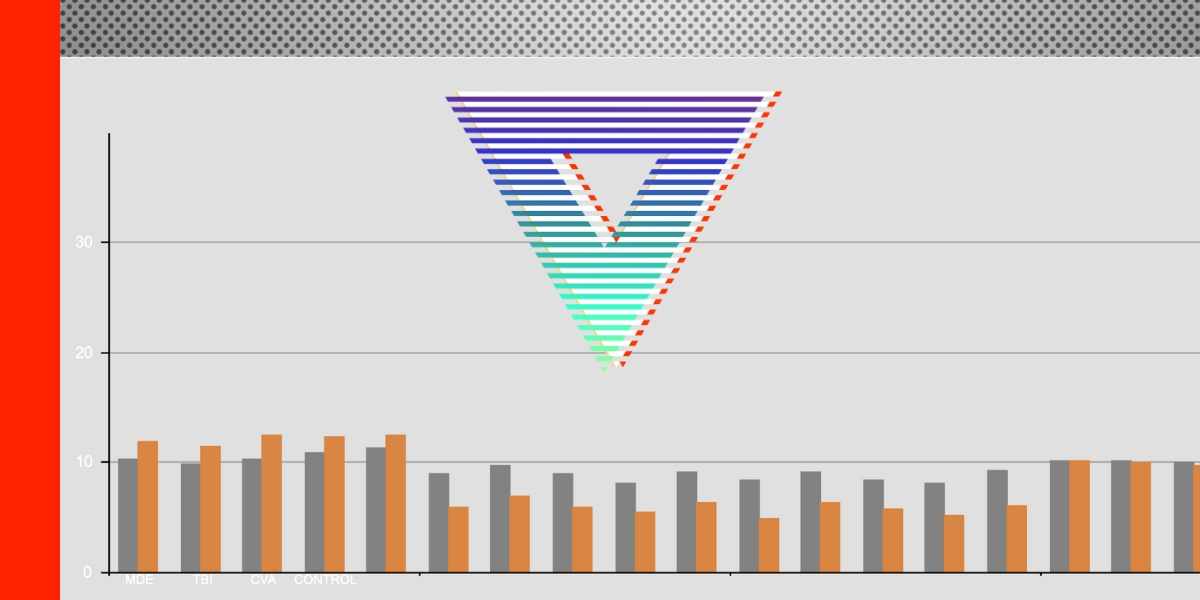
The point here is to use it briefly, to make time for another less potentially harmful intervention. Similarly, when considering CCP, targets and protocols use population averages.
No single optimal CCP exists across all patients. So, clinicians need a rationale way to titrate treatment to physiology.
David suggests using graded thresholds to escalate treatment in an individualised way. Underlying these principles is good detection and minimisations of treatment harm.
Underlying all of these principles is a grounding in the data and the utilisation of this data to effectively communicate with families.
By doing this you can deliver the treatment and aim for the outcomes deemed most acceptable by the patient and their loved ones.
Managing ICP in Traumatic Brain Injury: David Menon
For more like this, head to our podcast page. #CodaPodcast
David Menon
David Menon is Professor and Head of the Division of Anaesthesia, Principal Investigator in the Wolfson Brain Imaging Centre, and Co-Chair of the Acute Brain Injury Programme at the University of Cambridge. In 2013 he was re-appointed as NIHR Senior Investigator as one of the NIHR’s pre-eminent researchers.
He trained in Medicine, Anaesthesia and Intensive Care at the Jawaharlal Institute in India, Leeds General Infirmary, The Royal Free Hospital and Addenbrooke’s Hospital, and was an MRC Research Fellow at the Hammersmith Hospital prior to coming to Cambridge.
In 2006 he was appointed to the British Oxygen Professorship at the Royal College of Anaesthetists. He is Co-Chair of the Executive Board of the European Brain Injury Consortium, is a Founding Fellow of the Academy of Medical Sciences, and a Professorial Fellow in the Medical Sciences at Queens’ College, Cambridge.
He was the first Director of the Neurosciences Critical Care Unit (NCCU) at Addenbrooke’s Hospital, Cambridge, where he established the first recognised training programme for specialist neurocritical care in the UK. Protocols developed in the Addenbrooke’s NCCU have been shown to improve clinical outcome in severe head injury and rationalise the management of acute intracranial haemorrhage.
Professor Menon’s research interests include neurocritical care, secondary brain injury, neuroinflammation, and metabolic imaging of acute brain injury. He has also published on the physiology of coma and the vegetative state, and on mechanisms of anaesthetic action in the brain. In recent years he has represented the UK intensive care community in discussions regarding the impact of evolving legislative changes on research in critical care and emergency medicine.